Simple and fast insurance payments.
POWER UP YOUR PRACTICE
One platform. Better outcomes.
Save time, get paid faster, and grow your practice — all with one powerful platform. Our first-of-its-kind partnership with Zelis revolutionizes the way providers process insurance reimbursements, fueling efficiency and growth.
Benefit from:
Together, Bridge™ Payments and Zelis cut reimbursement processing time in half. The advanced integration is designed to shorten payer payment processing cycles and fuel practice growth. Practices pairing Bridge Payments and Zelis have reduced accounts receivable by up to 2 weeks.
Our technology automates receiving and processing payer payments, so you can focus on what matters most: delivering exceptional patient care. Experience up to 5x faster insurance reimbursement processing and save around 20 staff hours a month.
Say goodbye to manual data entry and hello to accurate and up-to-date claims data. Automated insurance reimbursement processing results in fewer data errors and protects your practice by providing a higher level of security for insurance claims payments.
Easily access standardized explanations of payments, down to the claim-level detail. Together, Bridge Payments and Zelis enhance transaction and cash flow visibility. Easily monitor your revenue cycle and identify areas for improvement.
Top Bridge™ Payments + Zelis features.
Everything you need for faster payments and a thriving practice.
Straight-Through Processing
One-click refunds
For quick payback of insurance and patient payments.
Sophisticated reporting
Greater visibility into your revenue cycle.
Full payment suite
More ways to pay like contactless and Text-to-Pay.
Online bill pay
Patients can pay from anywhere, 24/7.
Seamless payment posting
Directly into your EMR, EHR, PMS, in real time.
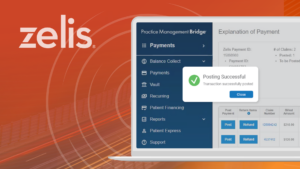
Revolutionizing the entire claims process.
Straight-Through Processing™ works quickly to get your practice paid and save your staff time. Here’s how it works:
- Zelis initiates a virtual credit card payment and standardized explanation of payments.
- Once approved, the funds settle into the provider’s bank account.
- The provider verifies the payment and posts to the PMS with one click.
Ready to experience faster payments?
Accelerate revenue cycles and save time with Straight-Through Processing from Bridge Payments and Zelis. Learn how easy processing reimbursements can be, saving you time, reducing practice risk, and minimizing accounts receivable. Schedule a demo today to see how Bridge Payments and Zelis can help you:
- Speed up payer reimbursement.
- Eliminate administrative tasks
- Reduce practice risk.
- Meet your revenue cycle goals.


